If you are suffering from chronic acid reflux or have been diagnosed or suspect you may have Barrett’s esophagus, you probably have a number of questions you want answered. Here are answers to some common questions people have regarding the condition:
Q: What causes Barrett’s esophagus?
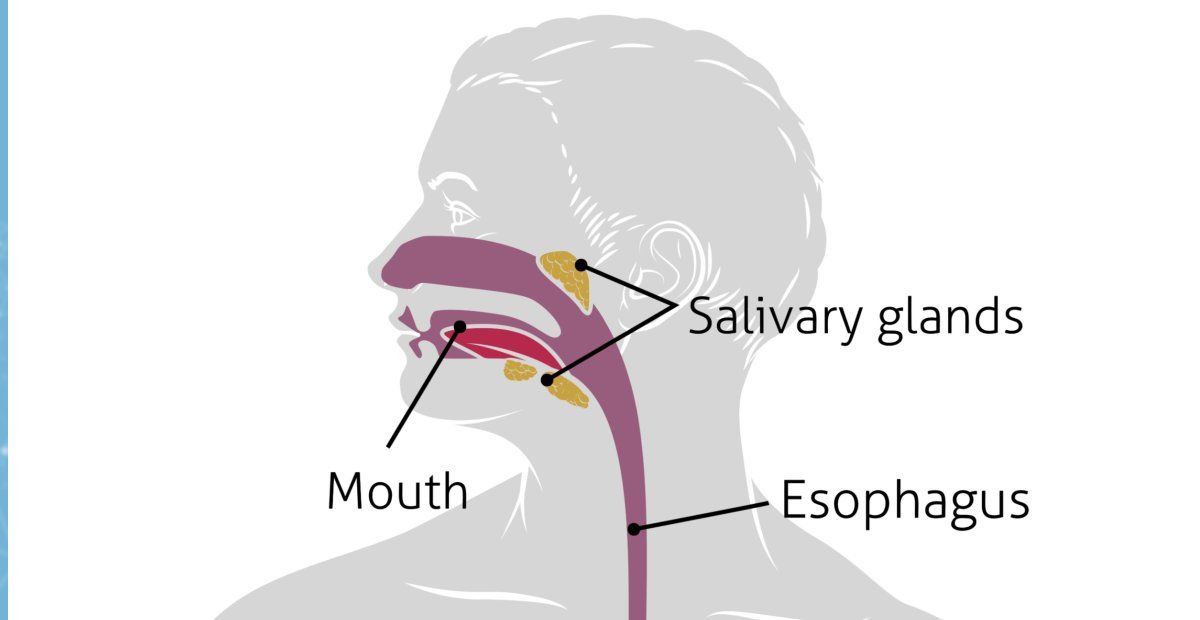
A: Barrett’s esophagus is usually a compilation of gastroesophageal reflux disease (GERD). It is when frequent acid reflux occurs in the esophagus, irritating and inflaming its lining. Chances of GERD are increased when someone is obese, has a hernia, is pregnant, has a tissue disorder like scleroderma, and other conditions. Acid reflux can particularly be aggravated by:
Over time, chronic acid reflux damage can change the tissue lining the lower esophagus — which is essentially what Barrett’s esophagus means.
Q: How often does Barrett’s esophagus become esophageal cancer?
A: Most people with GERD do not get Barrett’s esophagus, and only about 1% of people who have Barrett’s esophagus develop esophageal cancer. However, that 1% is fairly significant, when you realize that that is a 125 times higher risk of getting esophagus cancer than people without Barrett’s esophagus have. People diagnosed with Barrett’s esophagus should get regular screenings/endoscopy exams to ensure that cancer has not begun to develop.
Q: How is Barrett’s esophagus diagnosed?
A: An endoscopy test is used to diagnose and stage Barrett’s esophagus. In this test, one of our gastroenterologists put a thin tube with a camera down your throat to examine the lining of your esophagus. You will typically be sedated and anesthetized during the exam to reduce discomfort. If the doctor finds any changes in the lining of your esophagus that indicate Barrett’s esophagus, a tissue sample will be taken and a biopsy under a microscope will be conducted, to check for cancer. This test gives us the information we need to diagnose whether or not you have Barrett’s esophagus, how far along the damage is, and the likelihood of it becoming cancerous and spreading to other parts of the body.
Q: What are the stages of Barrett’s esophagus?
A: There are five stages of Barrett’s esophagus:
Non-dysplastic (no cancerous tissue whatsoever)
Low-grade dysplasia (minor cell changes found)
High-grade dysplasia (Extensive cell changes, but not yet cancer)
Noninvasive cancer
Invasive cancer
Q: What is the treatment for Barrett’s esophagus?
A: One of the benefits of getting treatment for Barrett’s esophagus at Northeastern Gastroenterology Associates is that every one of our providers has been thoroughly trained and are experienced in treating this condition. Depending on the severity of your symptoms, we may recommend medications, lifestyle changes, or even surgery. Our goal is to provide you with treatment that will reduce your risk of cancer, make you feel better, and keep the disease from getting worse. Some specific endoscopic therapies that may be suitable for people with Barrett’s esophagus that is not yet strongly cancerous include:
Argon plasma coagulation — This technique involves the direction of argon gas through an endoscope to destroy potentially cancerous cells with an electric current.
Radiofrequency ablation — Radio waves are used to destroy abnormal tissue.
Cryoablation — This technique involves a gastroenterologist applying a very cold liquid or gas to the abnormal tissue to freeze and destroy it.
Photodynamic therapy — A light-sensitive drug and laser-therapy is conducted to destroy the abnormal cells.
Endoscopic mucosal resection — This procedure involves the shaving off of the abnormal tissue.
The gastroenterologists at Northeastern Gastroenterology Associates have had excellent results using these procedures. Contact us to learn more about how we can diagnose and treat Barrett’s esophagus.
Q: What treatment would I get if I got invasive cancer?
A: Treatment for esophagus cancer may involve surgery or a combination of surgery, chemotherapy, and radiation.
Q: Can Barrett’s esophagus heal itself?
A: Lifestyle changes such as eliminating chocolate, spicy foods, fatty foods, caffeine, etc. can lead to healing from the condition. Medications also can help, such as proton pump inhibitors and antacids.